Bladder conditions can be debilitating and you might feel isolated and like you are the only one suffering, but it’s important to remember you are not. It is estimated that 14 million¹ people in the UK are living with bladder problems, so you are not alone and there is a wealth of information and support available.
Self-administration help
Videos and information to support you with self-administration.
Bladder conditions
Further information on IC/BPS
and recurrent UTIs.
Blog and downloads
In-depth articles, and helpful guides and diaries available to download and print.
Bladder Matters
Join our
social media community
Further support
Links to charities
and further information.
Bladder conditions
What is it?
A chronic bladder condition characterised by mild discomfort, pressure, tenderness or intense pain in your bladder and pelvic area. These symptoms often persist for many weeks.
How common is it?
It usually affects women in their 40s and is thought to occur in 1 in 50 women⁵.
What are the symptoms?
Pain: The pain associated with IC can be felt in the lower abdomen, pelvis, vagina and urethral tube (the tube which connects the bladder to outside of the body), and is often associated with sexual intercourse. Male IC patients may also experience pain in their testicles and painful ejaculation.
Urgency: The sense of needing to urinate immediately can also be accompanied by discomfort due to sensations of pressure and pain.
Frequency: In severe cases, day and/or night-time frequency of urinating can be up to 50 times per day. An increase in frequency can be the only presenting symptom in the early stages of the condition. Often, only a small amount of urine is passed each time.
The symptoms usually come and go, with some flare-ups lasting days, weeks or months.
What are the risk factors?
To date, the cause of interstitial cystitis/painful bladder syndrome is unknown. Some theories regarding its cause include:
- Damage to your bladder tissue, which may allow substances in the urine to irritate the bladder and nerves
- A problem with the pelvic floor muscles that control peeing
- A type of immune reaction
How is it diagnosed and treated?
Diagnosis can take time as the symptoms are similar to other bladder conditions such as an overactive bladder, bacterial cystitis or chronic UTI. Diagnostic tests such as urodynamics or cystoscopy might be used. Unlike more common forms of cystitis, IC is not caused by bacterial infection and therefore does not respond to antibiotic treatment.
As the exact cause of IC is unknown, there is no cure. Some treatment options are available however, that can reduce the severity of the symptoms you may be experiencing and lower the impact that IC has on your quality of life. These options range from taking oral medications to reduce the individual symptoms, to having a product instilled into your bladder (eg. iAluRil) in an attempt to re-build the waterproof protective lining of your bladder. By discussing your condition with your Doctor, Nurse or Urologist you will be able to evaluate each option and determine which treatment will work best for you.
How can it affect your life?
Because of the frequent and urgent need to urinate, many IC/BPS patients’ lives revolve around planning where the nearest toilet is. This can also cause sleep deprivation. The lack of any obvious physical disability results in some patients feeling socially isolated and misunderstood, which can lead to depression.
Self-administration videos
Use our nurse-led training videos to help you perform intermittent self-catheterisation safely,
or to effectively use the iAluadapter for catheter free administration of your iAluRil.
Self-administration video for women
Self-administration video for men
BPS/IC self-management tips
Whilst formal treatment for BPS may take the form of bladder instillations, oral medication, surgery or nerve stimulation,
there are some things you can do yourself to help control the symptoms.
It is well known that diet can help in the management of BPS. Spicy food and caffeine should be avoided, as should acidic foods, as these can increase the acidity of your urine which can cause irritation. Whilst you may need to eliminate certain foods, it is still important to try and maintain a healthy, well balanced diet.
Foods to avoid: alcohol, carbonated drinks, caffeine, fruit juice, aged cheese, tomatoes, yogurt, pickles, spices, sugar and sweeteners.
Not all foods will have the same affect for BPS patients so try keeping a food diary to see which foods cause flare-ups, and try eliminating one thing at a time.
Coping with BPS can be stressful, and reducing this stress has helped some BPS sufferers manage their condition better. This can be achieved in a number of ways including meditation, breathing exercises or simply seeing friends and family or having a warm bath. Find the best way that works for you and that fits into your lifestyle and routine; that way, you’re more likely to keep it up.
Planning ahead is a big part of coping with BPS. If you’re heading out and about, check where the nearest loos will be and find a route (either on foot or in a car) which has plenty of suitable toilet stops if needed, or places just to sit and rest. Take into account any extra time this may take too. Check the menu options if you’re eating out, and if you’re seeing friends, make sure they are aware of any dietary requirements.
Keeping active is vital if you suffer from BPS and gentle exercise such as walking, tai chi, yoga and pilates can be beneficial for some BPS patients. Nowadays, there are plenty of online classes if you would prefer to be in the comfort of your own home. Yoga and pilates will also help strengthen your pelvic floor muscles which might provide some symptom relief.
Blog
GAG therapy research
Learn how research into GAG therapies is undertaken and how past and present studies help to explain the efficient, reliable nature of iAluRil and its logical use in the treatment and management of IC/BPS and rUTIs.
The GAG Layer- by Maike Eylert, Consultant Urologist
Maike Eylert, Consultant Urologist at Aneurin Bevin University Health Board, explains what the glycosaminoglycan (GAG) layer is and how GAG replenishing therapy can help when it becomes damaged.
Downloads
The resources below are available for your information and record keeping. Click on them to download.
Patient information
Patient information leaflet
This leaflet will provide you with all the information you need to understand what iAluRil is, how it is administered, how long treatment would typically last and what to expect in terms of potential side effects.
Please speak to your Healthcare Professional for a copy.
Patient Diary
Use this to keep a record of your instillations.
The information you record will be of use to your clinician.
Please speak to your Healthcare Professional for a copy.
Patient Food Diary
This diary can be used to find out which foods might be causing a flare up of your interstitial cystitis/bladder pain syndrome symptoms, and help highlight what should be avoided.
ISC information
ISC step by step instructions for Women
A handy step by step guide to administering your iAluRil via a catheter.
ISC step by step instructions for Men
A handy step by step guide to administering your iAluRil via a catheter.
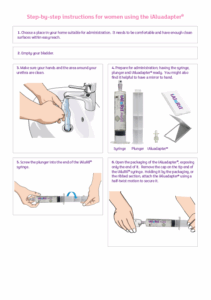
iAluadapter information
iAluadapter step by step instructions for Women
A handy step by step guide to administering your iAluRil using the iAluadapter.
iAluadapter step by step instructions for Men
A handy step by step guide to administering your iAluRil using the iAluadapter.
Join the Bladder Matters community
A supportive community for patients suffering from bladder conditions
- Useful tips
- Relatable stories
- Background science
- iAluRil info
Further support
Click the links below to leave iAluRil.co.uk and find out more information about IC/BPS, rUTIs and the support and help available to you.
By using the links below you will leave the iAluRil website and be re-directed to an external site;
Aspire Pharma is not responsible for the content on external websites.
References
Reference 1
NHS England: https://www.england.nhs.uk/2015/11/continence-care/ (Accessed October 2024)
Reference 2
NHS, Interstitial Cystitis. Available at: https://www.nhs.uk/conditions/interstitial-cystitis/ (Accessed October 2024)
Reference 3
Hopkins Medicine, Interstitial Cystitis. Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/interstitial-cystitis#:~:text=Interstitial%20cystitis%20(IC)%20is%20an,It%20is%20a%20chronic%20disorder. (Accessed October 2024)
Reference 4
NHS, UTIs. Available at: https://www.nhs.uk/conditions/urinary-tract-infections-utis/ (Accessed October 2024)
Reference 5
Patient. Painful bladder Syndrome (interstitial cystitis) https://patient.info/health/painful-bladder-syndrome-interstitial-cystitis (Accessed October 2024)
Reference 6
London Urology Specialists: https://www.londonurologyspecialists.co.uk/urinary-tract-infection/ (Accessed October 2024)
IAL1010244H11_FEB2026